Thyroid and Hair Loss: The Connection Explained
You notice more strands in your brush than usual. Your ponytail feels thinner. The shower drain seems to clog daily. Unexplained hair loss is a distressing and confusing experience, one that can leave you feeling helpless and searching for answers. While there are many potential culprits, from stress to nutrient deficiencies, one often-overlooked source lies in a tiny, butterfly-shaped gland in your neck: your thyroid.
The link between thyroid dysfunction and hair loss is profound and, thankfully, well-documented in the medical world. If your hair is thinning and you can’t pinpoint why, understanding this connection could be the key to unlocking the solution. This isn’t about a bad hair day; it’s about a fundamental signal from your body that something is out of balance. In this comprehensive guide, we will demystify the relationship between your thyroid and your hair, exploring the mechanisms, the signs to look for, and most importantly, the path toward diagnosis, treatment, and recovery.
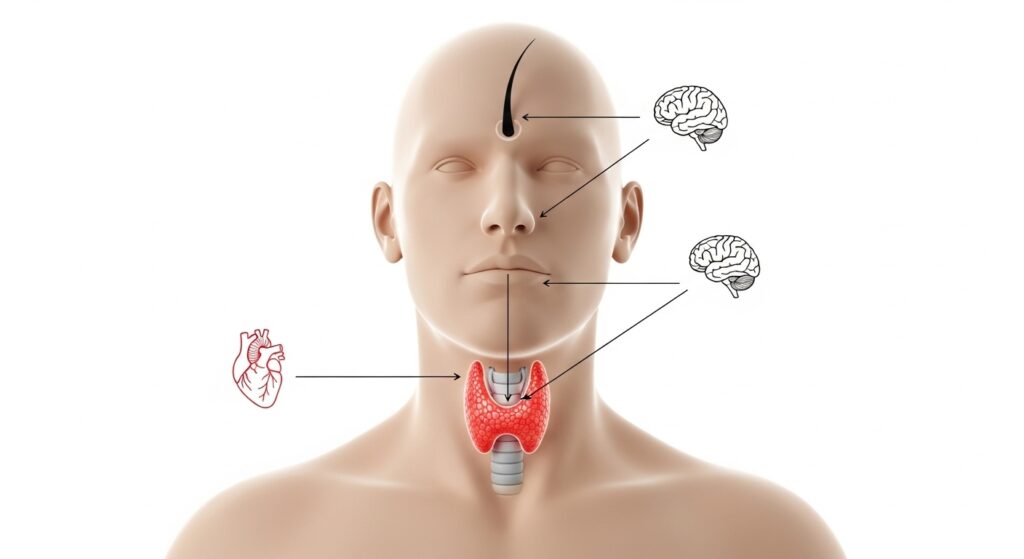
What is the Thyroid and What Does It Do?
Before we dive into hair loss, it’s crucial to understand the master gland at the center of it all. Your thyroid is a small, powerful organ located at the front of your neck. Think of it as your body’s thermostat and metabolic control center. It produces two primary hormones: Thyroxine (T4) and Triiodothyronine (T3).
These thyroid hormones travel through your bloodstream to every tissue and organ, influencing everything from your heart rate and body temperature to your energy levels and, critically, your hair growth cycle. They help regulate the speed at which your body’s cells work. When your thyroid is functioning optimally, it produces just the right amount of hormones to keep your systems in harmony. This state of balance is known as euthyroidism.
The Hair Growth Cycle: A Delicate Balance
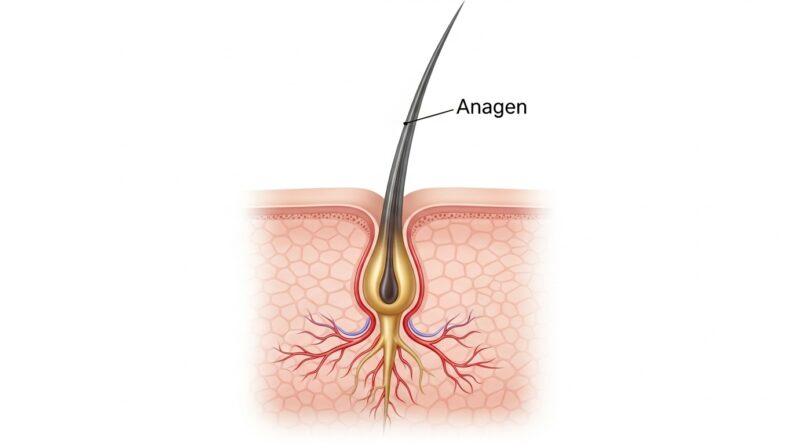
To grasp how the thyroid disrupts hair health, we must first understand how hair grows normally. Your hair follicles don’t continuously produce hair; they operate in a meticulous, multi-stage cycle:
Anagen (Growth Phase): This is the active phase where cells in the hair root divide rapidly, forming new hair. This phase can last for several years, and about 85-90% of your hair is in this stage at any given time.
Catagen (Transition Phase): A short, transitional period lasting about two weeks. Hair growth stops, and the outer root sheath shrinks and attaches to the root of the hair. This is a sort of “resting” period before the final stage.
Telogen (Resting & Shedding Phase): This is the final phase, lasting around three months. The hair follicle is completely at rest, and the club hair (the fully formed hair) is eventually shed. Normally, we shed 50-100 telogen hairs a day.
This cycle is a finely tuned process, and it is exquisitely sensitive to internal changes. Any significant hormonal shift, including those caused by thyroid disorders, can shock the system and disrupt this delicate rhythm.
How Thyroid Disorders Specifically Cause Hair Loss
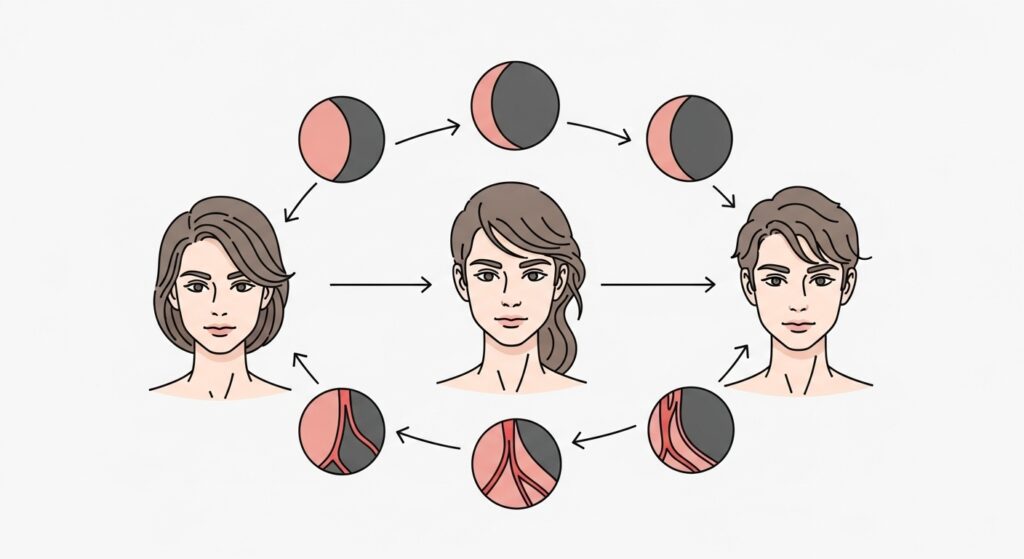
Both an overactive and an underactive thyroid can lead to hair loss, albeit through a common final pathway. The primary problem isn’t that the hair follicle is destroyed; it’s that its growth cycle is severely disrupted.
Hypothyroidism (Underactive Thyroid): When your thyroid doesn’t produce enough hormones, your body’s metabolic processes slow down. This includes the rate of cell division in your hair follicles. The anagen (growth) phase shortens, and a higher-than-normal percentage of hairs prematurely enter the telogen (resting) phase. The result is a condition called telogen effluvium—a diffuse shedding of hair all over the scalp, rather than in specific bald patches.
Hyperthyroidism (Overactive Thyroid): Conversely, an excess of thyroid hormones speeds up your metabolism. This can paradoxically also trigger telogen effluvium. The theory is that the accelerated metabolic rate pushes hair follicles into the resting phase too quickly to conserve energy for other, more critical bodily functions. The rapid cell turnover may also produce weaker, more brittle hair that breaks easily.
In both cases, the hair loss is typically diffuse, meaning it affects your entire scalp rather than causing discrete bald spots. You might also notice changes in the hair’s texture. With hypothyroidism, hair often becomes dry, coarse, and brittle. With hyperthyroidism, hair can become fine and soft.

What Does Thyroid-Related Hair Loss Look Like?
Identifying the pattern and characteristics of your hair loss can provide important clues. Thyroid-related hair loss has some distinct hallmarks:
Diffuse Thinning: The most common sign is a general thinning of hair across the entire scalp. Your part might look wider, or your ponytail may feel significantly thinner.
Hair Shedding: You may notice an excessive amount of hair falling out daily—on your pillow, in the shower, or in your hairbrush.
Loss Beyond the Scalp: While the scalp is most affected, some people experience thinning of hair on the outer edges of their eyebrows (a sign known as madarosis, more common in hypothyroidism), and even body hair.
Texture Changes: As mentioned, the hair itself may change. It can become dry, straw-like, and difficult to manage (hypothyroidism) or unusually fine and soft (hyperthyroidism).
It’s important to note that hair loss is often a delayed symptom. It typically begins to appear several months after the onset of the thyroid disorder itself, and similarly, it can take months for hair to recover once treatment has begun.

Getting a Diagnosis: It’s More Than Just TSH
If you suspect your thyroid might be the culprit, the first and most critical step is to see a healthcare provider. Self-diagnosing and supplementing without guidance can be dangerous.
Your doctor will likely start with a blood test. However, a comprehensive thyroid panel is key. While the Thyroid-Stimulating Hormone (TSH) test is the standard screening tool, it doesn’t always tell the whole story. A full evaluation should also include:
Free T4 and Free T3: These measure the actual levels of active thyroid hormones circulating in your blood.
Thyroid Antibodies (TPO and TgAb): These tests check for autoimmune activity, which is the most common cause of thyroid dysfunction (Hashimoto’s disease for hypothyroidism, Graves’ disease for hyperthyroidism).
Many people can have “normal” TSH levels but still experience symptoms because their T3 is low or they have high levels of thyroid antibodies. Advocating for a full panel can provide a much clearer picture.

Treatment and Recovery: The Path to Hair Regrowth
The single most effective treatment for thyroid-related hair loss is to treat the underlying thyroid condition. The goal is to restore your thyroid hormone levels to a normal, optimal range—a state known as euthyroidism.
For hypothyroidism, this typically involves daily hormone replacement medication, such as levothyroxine (Synthroid, Levoxyl, Tirosint). For hyperthyroidism, treatment options include anti-thyroid medications (like Methimazole), radioactive iodine therapy, or sometimes surgery.
Patience is absolutely essential. Hair grows slowly. Once you begin effective treatment and your hormone levels stabilize, the hair growth cycle needs time to reset. You will likely need to wait 6 to 12 months to see significant regrowth. The shedding should stop first, often within 3-6 months, before new, stronger hair begins to fill in.
During this period, supporting your body is crucial. Ensure you are eating a balanced diet rich in iron, zinc, selenium, and biotin—all vital for hair health. Some studies suggest that people with autoimmune thyroid disease may be more prone to nutrient deficiencies like iron-deficiency anemia, which can exacerbate hair loss.

Lifestyle and Supportive Care for Hair Health
While medical treatment is non-negotiable, certain lifestyle practices can support your journey to healthier hair.
Gentle Hair Care: Treat your hair with kindness. Avoid harsh chemical treatments, excessive heat styling, and tight hairstyles that pull on the follicles. Use a wide-tooth comb on wet hair to prevent breakage.
Stress Management: Chronic stress can independently cause telogen effluvium, compounding the problem. Incorporate stress-reducing activities like yoga, meditation, or daily walks.
Balanced Nutrition: Focus on a whole-foods diet. Key nutrients for hair include protein (hair is made of keratin, a protein), iron, omega-3 fatty acids, and vitamins D and B12.
Scalp Care: A healthy scalp is the foundation for healthy hair. Gentle scalp massages can help stimulate blood circulation to the follicles.
Be wary of “miracle” hair growth supplements that make bold claims. Always discuss any new supplements with your doctor, as some, like high doses of biotin, can actually interfere with thyroid blood test results.

When to See a Doctor and Key Takeaways
If you are experiencing persistent, unexplained hair loss, especially if it’s accompanied by other symptoms like fatigue, weight changes, feeling too cold or too hot, or changes in your mood, it is time to schedule an appointment with your doctor or an endocrinologist.
To recap, the connection between thyroid and hair loss is clear and significant. Your thyroid hormone is a master regulator of your hair growth cycle. When levels are too high or too low, it can shock your system, pushing a large number of hair follicles into a resting and shedding phase. The resulting hair loss is usually diffuse and can affect your entire scalp and body.
The journey back to healthy hair begins with a proper medical diagnosis and consistent treatment of the root thyroid issue. It requires patience, self-care, and a gentle approach. While the waiting period can be frustrating, know that for the vast majority of people, thyroid-related hair loss is temporary and reversible. By addressing the internal imbalance, you give your body, and your hair, the foundation it needs to heal and thrive once again.